Cancer is not just the result of “bad luck” or rogue cells. It often develops in the context of a dysfunctional internal terrain. The body’s environment that includes the immune system, detoxification organs, and inflammatory status.
Over a century ago, scientists likened cancer to a “seed” that needs the right “soil” to grow.
In other words, a tumor (the seed) will only thrive if the body’s “terrain” (the soil) is favorable.
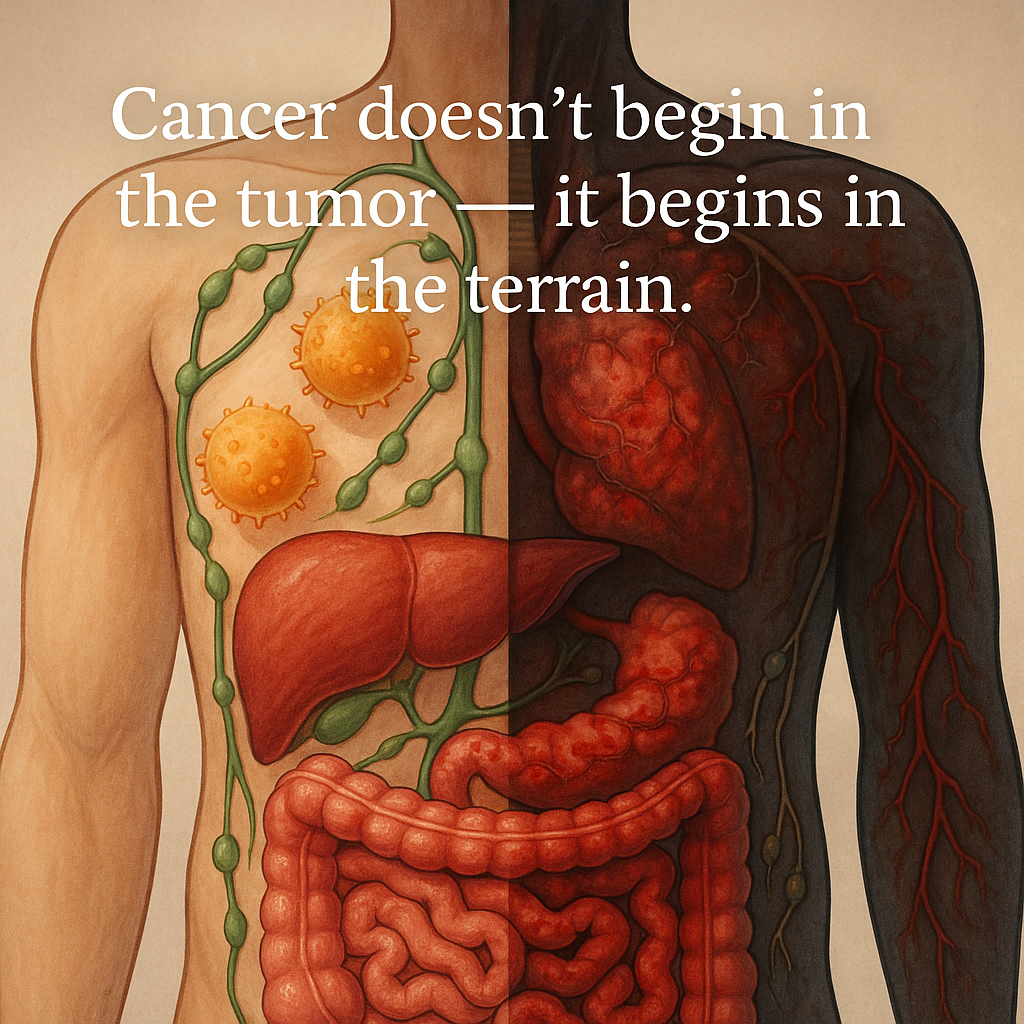
Modern research confirms that factors like immune weakness, toxin buildup, liver overload, and chronic inflammation can precondition tissues for cancer. This can happen long before any lump or lesion is detectable [1] [2].
This article will explore how these terrain imbalances impact health. These include immune suppression, lymphatic stagnation, impaired liver detoxification, and chronic inflammation with oxidative stress. They create a microenvironment ripe for DNA mutations and immune evasion by emerging cancer cells. This environment also supports new blood vessel growth (angiogenesis) and ultimately tumor progression.
We’ll also discuss why conventional treatments (surgery, chemotherapy, radiation, etc.) often fail to provide lasting cures if these underlying terrain issues aren’t addressed.
Finally, we highlight science-backed natural and lifestyle strategies to restore a healthy terrain. These strategies improve immune resilience, promote lymphatic flow, aid liver detox, and lower inflammation. They can benefit everyone, including those in African or low-resource settings, to prevent cancer or its recurrence.
Immune Suppression: When Immune Surveillance Fails
The immune system is one of the body’s primary defenses against early cancer. It includes the activity of lymphocytes, like T cells and natural killer cells. These cells constantly patrol for abnormal (mutated) cells.
Under healthy conditions, this immune surveillance can remove precancerous cells before they multiply [3] [4]. In fact, there is compelling evidence. The immune system can identify nascent tumors. It can destroy them, acting as an “extrinsic tumor suppressor” in the body [5].
The immune system clears viruses that cause cancers. It directly recognizes stress signals or tumor antigens on emerging cancer cells. By doing so, it kills them before they form a detectable tumor [6].
However, if immune function is suppressed or weakened, this surveillance breaks down. Reduced lymphocyte activity can result from chronic stress, poor nutrition, certain diseases, or drugs. This reduction means mutated cells are more to escape destruction.
Clinical data show that people with immunosuppression have dramatically higher cancer rates. For example, organ transplant patients on immunosuppressive drugs have a 3- to 100-fold increased risk of developing certain malignancies [7]. Many of these are lymphomas caused by viruses. However, even solid tumors with no viral cause occur more frequently when the immune system is suppressed [8].
Similarly, individuals with HIV/AIDS or congenital immune deficiencies suffer more cancers than the general population [9]. These observations underline that a competent immune system is constantly nipping early cancers in the bud, whereas an impaired one allows abnormal cells to proliferate unchecked [10] [11]
Immune surveillance sometimes falters. Consequently, more DNA mutations can accumulate, as damaged cells aren’t being removed. Simultaneously, fledgling tumor cells begin to evolve ways to evade the immune response.
Tumors can induce local immune suppression by recruiting certain suppressor cells or releasing inhibitory signals. In essence, an immune-compromised terrain gives cancer a free pass to set itself up. This is one reason cancer incidence rises with age. Immune function tends to decline in older adults. T-cell activity is especially affected, reducing cancer-fighting vigilance.
Lymphatic Stagnation: Toxic Build-Up in Tissues
The lymphatic system is often overlooked. However, it is a critical part of the body’s terrain. It helps remove cellular waste, toxins, and abnormal cells. It’s a network of vessels and lymph nodes that works alongside the circulatory system. As fluid courses through tissues, it collects debris like dead cells, bacteria, and metabolic toxins. These are drained as lymph into lymph nodes. There, immune cells can filter out and destroy harmful contents.
In fact, Your body relies on your lymphatic system to remove waste, like bacteria, viruses, and toxins. It also eliminates abnormal cells that can lead to cancer. [12] Lymph nodes act as immunological “police stations.” They are where suspicious cells, including potential tumor cells, are presented to lymphocytes for elimination. [13] [14]. After filtering, the lymphatic fluid returns to the bloodstream. Eventually, wastes are excreted via the kidneys or liver [15] [16].
Unlike blood, lymph flow has no central pump and depends on muscle movement and breathing to circulate.
Physical inactivity, chronic dehydration, or damage to lymph vessels can lead to lymphatic stagnation – a sluggish flow of lymph. When lymph circulation is poor, tissues may accumulate excess fluids and waste products. This stagnant environment is problematic for several reasons:
- Buildup of Toxins and Waste: Stagnant lymph means cellular toxins linger longer in the tissues. Metabolic by-products are not flushed out quickly. These substances can irritate and inflame local cells, contributing to DNA damage over time. For example, carcinogenic compounds might not be cleared efficiently, giving them more opportunity to induce mutations in cells.
- Reduced Immune Surveillance: If lymph flow is impaired, fewer immune cells traffic through the area. Disruptions of lymphatic function compromise immune function [17]. Normally, dendritic cells carry antigens from tissues to lymph nodes via lymphatic vessels to activate T-cells. Poor lymphatic drainage can thus isolate a tissue from immune oversight. This allows abnormal cell clones to grow without prompt immune attack.
- Hypoxia and Poor Nutrient Exchange: Edematous (fluid-logged) tissues can become poorly oxygenated. Low oxygen (hypoxia) and poor nutrient removal lead to the growth of aggressive cells. These cells thrive in such conditions. Many cancers flourish in hypoxic, acidic environments. These conditions can also trigger angiogenesis (growth of new blood vessels). The body attempts to improve oxygen delivery. Unfortunately, tumors hijack this process to feed themselves.
One extreme illustration of lymphatic stagnation contributing to cancer is Stewart-Treves syndrome. It is a rare angiosarcoma (cancer of blood/lymph vessels). This cancer arises in chronically lymphedematous tissue. Women who develop severe arm lymphedema after breast cancer surgery may experience long-term fluid stagnation. This stagnation, due to lymph node removal, can lead to this aggressive cancer. Inflammation associated with the condition worsens the risk in the swollen arm[18]. This syndrome, though rare, underscores that long-standing lymphatic congestion and inflammation can directly foster malignancy.
Even on a smaller scale, maintaining lymphatic flow is clearly important for cancer prevention.
A study by MD Anderson Cancer Center emphasizes that every step you take helps lymph do its job [19]. Muscle contractions push lymph fluid along. This action allows the lymph to be filtered. If one’s lifestyle is very sedentary, lymph stagnates. The result is like a stagnant pond versus a flowing stream: the former breeds disease.
In a stagnant terrain, toxins and damaged cells accumulate. Local immune defenses wane. This sets the stage for cancerous cells to emerge. They are not promptly eliminated.
Liver Overload: Impaired Detoxification and Carcinogen Buildup
The liver is the body’s chemical processing plant – detoxifying countless compounds that we ingest or that result from metabolism. This includes neutralizing potential carcinogens (from food, environment, or cigarettes) and metabolizing hormones.
A healthy liver keeps the blood relatively clean of toxins and maintains hormone balance. Conversely, an overburdened or dysfunctional liver allows toxins to accumulate and circulate. This accumulation contributes to DNA damage. It also causes chronic immune irritation throughout the body.
When the liver’s detox capacity is exceeded – whether by excess toxin exposure (e.g. alcohol, aflatoxins in moldy foods, industrial chemicals), poor nutrition (lacking antioxidants and cofactors needed for detox enzymes), or liver disease (hepatitis, fatty liver) – the result is a backlog of harmful substances. These substances can directly attack DNA or generate oxidative stress, increasing mutation rates.
For example, research shows that if the two-step liver detox process becomes unbalanced, there is fast Phase I activation of toxins. There is not enough Phase II conjugation to remove them. As a result, reactive intermediates build up, leading to inflammation and cell damage [20]. Chronic inflammation and cell injury in the liver or other organs can then kick-start cancer development.
Moreover, the liver plays a crucial role in metabolizing hormones and supporting immune function. If the liver isn’t clearing hormones properly, hormonal imbalances can occur that fuel certain cancers. Excess estrogen can accumulate in the body when liver function is sluggish. This condition of estrogen dominance is linked to a higher risk of breast and prostate cancers [21]. A well-functioning liver helps prevent such hormone-driven tumor growth by keeping hormones in check [22] [23] .
The liver also hosts specialized immune cells called Kupffer cells. These cells filter the blood coming from the gut. They destroy microbes and tumor cells that might enter the circulation.
If the liver is overloaded with toxins, this immune function can weaken. As one integrative medicine source explains, “when the liver is overwhelmed with toxins, its defense system weakens. This allows harmful cells to evade detection.”[24]
In other words, an overloaded liver means both more carcinogens in the body and a dampened immune surveillance.
Terrain dysfunction in the liver often correlates with systemic issues:
- Chronic liver inflammation (hepatitis, NASH from obesity) produces cytokines and free radicals that can initiate cancer in the liver (e.g. hepatocellular carcinoma) [25]. In Africa and Asia, for example, chronic hepatitis B and C infections lead to ongoing liver inflammation. This results in oxidative stress, which greatly increases liver cancer risk.
- If the liver cannot keep up with detoxification, carcinogenic substances like nitrosamines, mold toxins, or pollutants remain longer in the body, raising the likelihood they will damage cells in vulnerable tissues (like the colon, breasts, etc.).
- A sluggish liver also leads to high oxidative stress levels in the blood (due to poor clearance of free radicals and less production of antioxidants like glutathione). This systemic oxidative stress can hit many organs, sowing the seeds of mutation.
In short, a terrain with an “overworked” liver is fertile ground for cancer. It’s like a filter that hasn’t been cleaned – impurities start to leak through. Without addressing liver overload, one might remove a tumor, but the body remains steeped in the same carcinogenic pressures that caused the first cancer.
Chronic Inflammation and Oxidative Stress: Fertile Soil for Mutation and Tumor Growth
Chronic inflammation and oxidative stress are hallmark features of a pro-cancer terrain.
In a healthy scenario, inflammation is a short-term (acute) response to injury or infection that resolves once healing is done. But when inflammation becomes chronic and smoldering, it creates a dangerous microenvironment in tissues. This environment is rich in DNA-damaging molecules, growth signals, and blood vessel-forming factors. These factors can initiate and accelerate cancer development [26].
Scientists now recognize that an inflammatory microenvironment is a hallmark of nearly all cancers. This includes those not obviously caused by an infection or irritant [27] . How does chronic inflammation make the body’s terrain cancer-friendly? Several mechanisms:
- DNA Damage from Free Radicals: Inflammation calls in white blood cells. These include macrophages that release reactive oxygen and nitrogen species (ROS/RNS). Their role is to destroy pathogens. If inflammation is ongoing, these ROS/RNS can continually bombard nearby healthy cells, causing DNA mutations. Oxidative stress from chronic inflammation can cause DNA damage. It activates oncogenes or inactivates tumor suppressor genes. This process essentially triggers the mutation cascade that leads to cancer [28]. Oxidative stress also causes incorrect DNA repair, genomic instability, and telomere shortening – all of which favor cancerous transformation [29].
- Pro-Proliferative and Pro-Angiogenic Signals: Inflamed tissues are flooded with cytokines (like interleukins, TNF-α) and growth factors (like VEGF). These signals tell cells to proliferate (in an attempt to heal) and stimulate new blood vessel growth. A cell that has already acquired a mutation giving it a growth advantage can exploit these signals to grow into a tumor mass faster. Chronic inflammation effectively “induces angiogenesis and malignant growth” in incipient tumors [30]. VEGF induced by inflammation helps tumors establish a blood supply (angiogenesis), while other factors suppress apoptosis (normal cell death), letting damaged cells survive when they shouldn’t.
- Immune Suppression in the Tumor Microenvironment: Paradoxically, while an inflamed environment starts with an active immune response, chronic inflammation often leads to a state of immune tolerance or exhaustion in the tissue. Certain immune cells (like myeloid-derived suppressor cells and M2-type macrophages) accumulate and actively suppress killer T-cells in chronically inflamed tissues. In fact, chronic inflammation is involved in immunosuppression, providing a microenvironment favorable for tumor development and metastasis [31]. Essentially, long-term inflammation can flip the immune system to a dysfunctional state that protects emerging cancer cells from immune attack. For example, inflammatory conditions like ulcerative colitis can lead to colon cancer partly because constant inflammation disrupts normal immune surveillance in the colon.
- Tissue Remodeling and Invasion: Chronic inflammation often entails fibrosis (scar tissue formation) and the activation of enzymes that remodel the tissue matrix (like MMP enzymes). This can make it easier for mutated cells to invade neighboring tissues and eventually metastasize. The terrain becomes literally “softer” for tumor spread.
Many well-known cancer risk factors operate via chronic inflammation and oxidative stress. For instance:
- Infections: Persistent infections such as H. pylori in the stomach, hepatitis B/C in the liver, HPV in the cervix, or schistosome parasites in the bladder all cause years of inflammation in the affected organs. This greatly increases the risk of gastric cancer, liver cancer, cervical cancer, and bladder cancer respectively [32] . In sub-Saharan Africa, infection-driven inflammation is a major contributor to cancers (e.g., liver cancer from hepatitis, Kaposi sarcoma from KSHV in HIV patients).
- Obesity: Obesity is characterized by a chronic low-grade inflammatory state; fat tissue produces inflammatory cytokines and also causes elevated oxidative stress. This is why obesity is linked to at least 12 types of cancer [33]. The excess nutrients and adipose-induced hormones (like insulin, leptin) further create pro-growth, pro-inflammatory conditions systemically.
- Smoking and Pollution: Tobacco smoke introduces numerous free radicals and toxic chemicals with every breath, directly causing DNA mutations (oxidative damage) and triggering lung inflammation. Long-term smokers essentially bathe their lung tissue in oxidative stress, explaining why lung cells accumulate multiple mutations leading to cancer. Similarly, exposure to air pollution or industrial chemicals can cause chronic inflammatory responses in organs (e.g. silica dust in lungs leads to inflammation and lung cancer).
In summary, chronic inflammation and oxidative stress act as a “fertile soil” for cancer seeds. They increase mutation rates. They suppress anti-tumor immunity. They promote blood supply to emerging tumors. They facilitate tumor invasion. Addressing chronic inflammation in the body is important. Reducing it is a key part of correcting the terrain to make it inhospitable to cancer.
The “Perfect Storm” Microenvironment – and How Conventional Treatment Misses It
A dysfunctional terrain, as we have seen, is characterized by immune weakness, toxic buildup, liver dysfunction, and chronic inflammation. These factors create the perfect storm for cancer to develop and thrive.
In this environment, cells accumulate genetic damage faster. The immune system fails to eliminate abnormal cells. Pro-cancer signals abound. Even the tissue structure becomes more inviting for tumor growth.
By the time a tumor is detectable, it is essentially the product of this broken terrain. The cancer has co-evolved with its microenvironment. It often hijacks inflammatory and immunosuppressive pathways to protect itself. Meanwhile, it pushes for more angiogenesis and growth.
Limitations of Conventional “Seed-Focused” Treatments
Modern conventional cancer treatments include surgery, chemotherapy, radiation, and newer targeted drugs. They have achieved many remissions. These treatments have saved lives, especially by removing or killing the main tumor (“the seed”).
However, these treatments typically focus on the tumor cells themselves, and not on the underlying soil (the patient’s internal environment). The dysfunctional terrain can remain even when the primary tumor is eradicated. As a result, this terrain can eventually allow cancer to return or a new cancer to form.
It’s well documented that many cancers, especially advanced ones, tend to recur after conventional therapy.
For example, patients with aggressive cancers may undergo surgery and chemotherapy, only to have microscopic cancer cells that survived treatment start growing again months or years later.
Why does this happen?
One reason is tumor heterogeneity and resistance. Within a given tumor, some cells are inherently resistant to treatment. Other cells may acquire resistance.
After chemo or radiation kills the susceptible cells, these resistant “seed” cells remain.
If the bodily environment – high in inflammation, low in immune surveillance, etc. – is still conducive, these surviving cells proliferate in the same old terrain, causing relapse. An international task force of scientists observed that most patients have a relapse after a few disease-free months. This occurs when they are on modern targeted therapies. This happens because tumors harbor therapy-resistant cells that escape. These cells find ways to keep growing [34]. In other words, you can cut down the weed. If you don’t change the soil, the weed—or another like it—will grow back.
Conventional treatments can also inadvertently worsen terrain factors in some cases.
Chemotherapy and radiation, for instance, are quite toxic. They can cause significant tissue damage. These treatments also suppress the immune system. Additionally, they create chronic inflammation as side effects.
Paradoxically, research has found that therapy-elicited chronic inflammation can promote treatment resistance and cancer progression [35] . For example, radiation removes a tumor mass. However, it leaves behind scarred, inflamed tissue. This is where new cancer seeds take root.
Chemo often drastically reduces white blood cell counts, impairing immune surveillance even further in the short term.
Some chemotherapies also elevate inflammatory cytokines or growth factors as a stress response, which might stimulate any remaining cancer cells. Furthermore, chemo cannot effectively kill cancer stem cells. These are a small subpopulation of cells in tumors. They are highly resistant and can regenerate the tumor.
These cancer stem cells “hide” during treatment and then drive recurrence later [36] [37].
They especially thrive if the patient’s systemic environment is still favorable to cancer (high oxidative stress, poor diet, etc.). Indeed, cancer stem cells are thought to be responsible for disease recurrence. They may also contribute to metastatic spread even after the primary tumor is removed [38].
Surgery, while crucial for removing solid tumors, also has limitations if terrain issues aren’t addressed.
Cutting out a tumor doesn’t alter the inflammatory or hormonal milieu that may have fed that tumor. This is why cancers like breast or prostate cancer can recur in the same area or as metastases elsewhere if one doesn’t also correct the systemic factors (diet, hormones, etc.) that contributed.
Surgery itself can cause lymphatic damage. This damage potentially leads to lymphedema and local immune deficits. Surgery can also trigger a wound-healing inflammatory response. In rare cases, this might stimulate any residual cancer cells to grow.
The bottom line is that conventional therapy treats the symptom (the tumor) more than the cause.
Traditional oncology has long considered cancer a cell-intrinsic genetic disease. Therefore, it focuses on killing tumor cells directly. However, multidrug resistance of cancer cells is a crucial reason for the low long-term efficacy of such therapy [39]. If the “soil” remains fertile – suppressed immunity, lots of toxins and inflammatory signals, etc. – then even a few surviving cancer seeds can sprout again. This situation also applies to second cancers. If someone’s terrain led to one cancer and nothing changes, there is a risk for other primary cancers later. The risk for subsequent primary cancers remains if conditions do not change.
Conventional treatments are often necessary and can be life-saving. For long-term success, they need to be paired with terrain-focused strategies. Consider it like repairing a crack in a wall. This shows tumor removal.
Nonetheless, not fixing the unstable foundation, which is the terrain, can cause the crack to reappear. In recent years, oncologists are increasingly acknowledging this. As a result, integrative oncology and survivorship programs have risen. These programs focus on diet, exercise, stress reduction, and other lifestyle factors to improve outcomes after conventional treatment.
In fact, it’s estimated that at least 50% of the most common cancers are attributable to lifestyle and environmental factors. These factors also strongly influence outcomes and recurrence [40]. It’s not “alternative” vs “conventional” – it’s about combining tumor-targeting treatments with terrain-targeting changes for the best long-term result.
Restoring a Healthy Terrain: Natural Strategies for Prevention and Healing
Correcting the body’s terrain is a powerful approach to cancer prevention and to supporting treatment.
Unlike expensive drugs, many terrain-focused interventions are low-cost or free and accessible even in low-resource settings – things like improving one’s diet, getting regular exercise, ensuring clean water and air, and managing infections.
Below, we outline evidence-based natural and lifestyle strategies to strengthen each key aspect of the terrain.
These measures can help prevent the initial breakdown that leads to cancer and also support the body in fending off recurrence if one has been treated. Importantly, these habits benefit overall health (reducing other diseases like diabetes and heart disease) and thus are doubly valuable in places with limited healthcare resources.
Strengthening Immune Surveillance Naturally
- Optimal Nutrition for Immunity: A diet rich in vitamins, minerals, and phytonutrients is critical for immune cell function. Deficiencies (for example, of vitamin D, C, zinc, or selenium) can impair lymphocyte activity. Emphasize a variety of fruits and vegetables, which provide antioxidants and bioactive compounds that support immune defenses. For instance, compounds in berries and leafy greens reduce oxidative stress and inflammation, indirectly bolstering immune cells. Sufficient protein is also important, since antibodies and immune cell receptors are made of protein.
- Regular Moderate Exercise: Consistent physical activity is one of the most potent natural immune boosters. Exercise mobilizes immune cells into the bloodstream and enhances circulation to patrol for threats. Research shows that moderate-intensity exercise increases natural killer (NK) cell activity and T-lymphocyte function [40], thereby improving the body’s ability to seek and destroy emerging tumor cells. Even a single bout of exercise can increase immune cell counts in circulation [41]. Aim for at least 30 minutes of moderate exercise (brisk walking, cycling, dancing, etc.) on most days. In cancer survivors, regular exercise has been linked to lower rates of recurrence, likely due in part to immune benefits. And in low-resource settings, “exercise” might simply mean utilitarian physical activity like walking to work, farming, or doing manual chores – all of which count.
- Adequate Sleep and Stress Management: Chronic sleep deprivation and unmanaged psychological stress elevate cortisol and other stress hormones that suppress immune function (particularly T-cell and NK cell activity). Make sleep a priority – adults generally need 7–9 hours of quality sleep. The body performs many repair and immune regulation tasks during deep sleep, including the peak of anti-tumor immune activity. Likewise, finding healthy outlets for stress (such as prayer/meditation, counseling, community support, yoga, or breathing exercises) can lower stress hormone levels and improve immune balance. Studies have shown that high stress can accelerate tumor growth (partly by dampening immunity), whereas stress reduction practices can enhance aspects of immune response.
- Avoid Immune-Draining Habits: Smoking, excessive alcohol, and drug abuse all weaken immune defenses. Smoking, for example, not only introduces carcinogens but also impairs the respiratory immune cells. Excess alcohol can reduce white blood cell counts and function. Limiting or eliminating these substances gives the immune system a better chance to stay vigilant.
- Prevent and Treat Chronic Infections: In many African and low-resource communities, infections like hepatitis B, HIV, HPV, malaria, and parasitic infestations are common and can chronically stimulate or depress the immune system. Vaccination is a critical tool here – for instance, widespread HBV vaccination has dramatically lowered liver cancer rates in countries that have implemented it, by preventing chronic hepatitis. Similarly, HPV vaccination in teens prevents the infections that cause cervical cancer. Treating conditions like HIV with antiretrovirals can help restore immune function and reduce AIDS-related cancers. On a community level, improving sanitation (clean water, controlling malaria and schistosomiasis, etc.) reduces the infectious burden that contributes to immune exhaustion and inflammation. This is as much a cancer prevention strategy as it is infectious disease control.
- Immunoregulatory Foods and Herbs: Certain foods and herbal supplements have evidence for modulating immunity. For example, mushrooms (such as shiitake, reishi, turkey tail) contain beta-glucans that can stimulate immune cells and are being researched for adjunct cancer therapy. Garlic is noted for immune-enhancing and antimicrobial properties. Turmeric (curcumin) and green tea, discussed more below, have antioxidant and immunomodulatory effects that could support immune surveillance [42]. Any addition should be evidence-based and used with consideration of individual health conditions, but generally a whole-foods diet with medicinal spices and herbs can contribute to a more resilient immune system.
Promoting Lymphatic Drainage and Detoxification
- Move Your Body (Reduce Sedentary Time): As mentioned, the lymphatic system relies on muscle contractions and body movement to circulate lymph. Regular exercise – even simple activities like walking, cycling, or dancing – will “pump” lymph fluid and prevent stagnation. “All these things stimulate lymphatic flow,” notes an MD Anderson physical therapist [43] . Activities that specifically emphasize full-body movement, like swimming or water aerobics, can be especially helpful (water pressure and muscle work both push lymph along) [44] . Even if one has a desk job, taking frequent short breaks to stretch or walk can keep lymph moving. In low-resource settings, many traditional lifestyles are naturally active (walking to get places, manual farming, etc.), which is beneficial – the key is to avoid the new trend of sedentary urban living as much as possible.
- Stay Hydrated: Lymph fluid is mostly water. Dehydration can make lymph thicker and flow more sluggishly. Ensuring you drink enough clean water throughout the day helps maintain proper lymph fluid volume and flow. Hydration also assists the kidneys in filtering blood and removing water-soluble toxins. A good guideline is the traditional 8 glasses (about 2 liters) of water per day, adjusted for climate (more in hot regions) and activity level. In areas where water access is an issue, consuming fluids through soups or hydrating foods (fruits, etc.) and making the most of available safe water is important for lymph and overall health [44] [45].
- Deep Breathing and Massage: Deep diaphragmatic breathing acts as a pump for the lymphatic system. The largest lymph vessel, the thoracic duct, empties near the neck. Breath movements create pressure changes that facilitate this action. Practicing deep breathing exercises daily can gently propel lymph. If someone shows signs of lymph stagnation or lymphedema, such as swelling in the limbs, a trained therapist can offer manual lymphatic drainage massage. This specialized massage can improve lymph flow and alleviate fluid buildup. In communities without access to specialized therapy, people can use self-massage techniques. Traditional practices like “dry brushing” involve lightly brushing the skin toward the heart. This method might also help stimulate lymph circulation in a low-tech way.
- Maintain a Healthy Weight: Obesity is a risk factor for lymphatic problems. Fatty tissue can physically compress lymph vessels. Obesity-induced inflammation can impair lymphatic function [46]. By maintaining healthy body weight through diet and exercise, one reduces those issues. As Dr. Chang of MD Anderson notes, “Obesity does cause damage to the lymphatic system.” It makes people more likely to experience lymphedema. It also contributes to cancer risk via inflammation [47]. Thus, weight control is key terrain care.
- Heat and Hydrotherapy: Some gentle therapies can assist lymph movement. Saunas or steam baths (if accessible) induce sweating. While sweat is not lymph, the heat causes blood vessels and lymph vessels to dilate. This potentially aids circulation of lymph and helps release some toxins through sweat. Contrast showers (alternating hot and cold water) cause expansion and contraction of blood vessels. They may also stimulate lymph vessel activity. These methods have a long history in traditional medicine for “detoxification,” though scientific research is still growing. Caution: these may not be suitable for everyone (e.g. those with heart conditions).
- Avoid Tight Clothing and Sedentary Postures: Believe it or not, extremely tight garments can hinder lymphatic drainage (for example, a very tight bra or belt might impede flow from an area). Wear comfortable clothing that doesn’t chronically constrict lymph-heavy regions. Also, try not to sit for many hours with legs crossed or in one position – this can pinch lymph channels. These small adjustments can ensure lymph fluid isn’t artificially blocked.
In summary, keeping the lymphatic “sewer system” flowing is essential for a clean terrain. It requires movement, hydration, and avoiding things that cause stasis. These cost little to nothing and can be implemented anywhere.
As one article succinctly put it: “Your body relies on your lymphatic system to remove waste…and every step you take helps it do its job.”[48] By consciously taking those steps (literally and figuratively), you help your internal environment stay clear of waste that could otherwise contribute to disease.
Supporting Liver Function and Detoxification
- Eat Liver-Supportive Foods: Food is perhaps the most powerful daily tool to enhance liver detox pathways. Certain foods contain nutrients that upregulate the liver’s ability to process toxins and reduce oxidative stress. For example, cruciferous vegetables like broccoli and cabbage are rich in indoles. Cauliflower and kale contain sulforaphane. These compounds boost Phase II detox enzymes in the liver [49]. This helps the liver neutralize carcinogens. Leafy greens (spinach, moringa, indigenous wild greens) provide chlorophyll and folate, aiding toxin binding and bile production [50]. Alliums like garlic and onions contain sulfur compounds. The liver uses these compounds for sulfation reactions in detox. This process supports glutathione production for Phase II [51] [52]. Turmeric (curcumin) and green tea have been shown to supply potent antioxidants. These antioxidants can lower liver inflammation. They reduce oxidative damage [53] [54]. In many African and Asian cuisines, these spices and teas are common – incorporating them regularly is beneficial. Finally, make sure adequate fiber by eating fruits, vegetables, and whole grains. Fiber helps capture toxins in the gut. These toxins are then excreted in bile and prevented from being reabsorbed.
- Stay Hydrated (for Kidney and Liver): We mentioned hydration for lymph, but it’s equally important for liver and kidney detox. The liver’s waste products are excreted in bile and leave the body through stool. These waste products are also sent to the blood. The kidneys then filter them into urine. Drinking enough water ensures the kidneys can flush out toxins efficiently. It also prevents constipation, ensuring toxins in bile leave the body promptly. Aim for at least 8 cups of water daily, and more if you sweat. In hot climates like many African regions, fluid needs can be higher. Clean water access is crucial. Advocacy for wells or filtration helps community health. It also reduces the toxin load from polluted water.
- Limit Alcohol and Avoid Toxins: One of the best gifts to your liver is minimizing its exposure to toxins. This reduces the burden on the liver. Excess alcohol is a direct liver toxin. It can cause fatty liver and cirrhosis over time. It also competes with other detox processes. When the liver is busy metabolizing alcohol, other toxins may accumulate. Limit alcohol to a moderate amount or none at all. Be mindful of environmental toxin exposures. For example, avoid smoking (as those chemicals go to the liver eventually). Use proper protection if you must handle pesticides or solvents at work. Choose clean foods when possible. In low-resource settings, some toxins come from old cooking/heating practices. This includes indoor coal or wood smoke. Improving ventilation or transitioning to cleaner stoves can reduce inhaled particulates. This reduces what the liver would have to clear from the bloodstream. Also, proper storage of grains can prevent mold (aflatoxin). Mold is a major liver carcinogen in some regions. Sun-drying crops and storing them in cool, dry conditions helps avoid this toxin.
- Improve Gut Health: The gut and liver are tightly linked (the “gut-liver axis”). A healthy gut microbiome can reduce the burden on the liver. For instance, certain gut bacteria can break down toxins or use up excess estrogen before they reach the liver. Conversely, an imbalanced gut can produce harmful metabolites that the liver then must detoxify. Eating fermented foods like yogurt, kefir, sour porridge, kimchi/sauerkraut, etc. introduces beneficial probiotics [55]. Consuming plenty of fiber from vegetables, fruits, legumes, and whole grains feeds good gut bacteria. It also helps trap toxins for removal [56]. A healthy gut means fewer endotoxins leaking into the blood, resulting in less liver inflammation and a stronger overall terrain.
- Regular Exercise: Exercise benefits the liver too. It improves blood circulation, so the liver gets a good supply of oxygen and nutrients. It can help prevent and reduce fatty liver by burning excess fat. Exercise makes you sweat. This process is a minor route of toxin elimination. Some heavy metals and waste can leave through sweat. As one source notes, “Movement improves circulation, helping toxins move through the body more efficiently. Sweating during workouts or sauna sessions can also help with toxin elimination.”[57] [58] Plus, exercise’s role in maintaining healthy weight prevents obesity-related liver strain. Aim for a mix of cardio and strength training weekly for liver (and whole body) health.
- Adequate Sleep and Down-Time: The liver performs a lot of its detox work during our rest, especially at night. In traditional medicine it’s often said the liver “recharges” between 1–3 a.m. While the specifics may vary, it’s true that poor sleep or shift-work schedules that disrupt circadian rhythms can affect liver metabolism and regeneration. Make sure to get quality sleep. Also, high stress levels can alter liver metabolism (stress hormones divert energy away from digestion/detox). Practices that reduce chronic stress – like meditation, leisure activities, and spiritual practices – indirectly benefit the liver. They do so by reducing inflammatory signals and allowing proper digestive function. “Chronic stress can increase inflammation,” which burdens the liver, so managing stress is part of terrain care [59].
- Herbal and Traditional Remedies: Around the world, various herbs are revered for supporting liver health. Milk thistle (silymarin) is one well-studied herb. It has antioxidant properties. It is used to help treat liver disease. There is some evidence it can reduce liver enzymes and fibrosis in hepatitis patients. Dandelion root, artichoke, and turmeric are other herbs believed to promote bile flow and antioxidant capacity. In African traditional medicine, plants like moringa, neem, or “Ugwu” (fluted pumpkin leaves) are used as blood and liver cleansers. Many of these plants are rich in vitamins and polyphenols. Science suggests they are beneficial. While herbal supplements should be used cautiously and ideally with professional guidance. However, incorporating culinary herbs and bitter vegetables that support the liver is generally positive. Even simple lemon water in the morning can gently stimulate the liver and gallbladder.
By eating clean and smart, we help the liver function optimally. Embracing healthy lifestyle habits also supports the liver’s performance. A well-supported liver will efficiently detoxify potential carcinogens. It will maintain balanced hormones. It will also quench much of the oxidative stress in our bodies. This transformation makes the internal terrain inhospitable to cancer.
Reducing Chronic Inflammation and Oxidative Stress
Chronic inflammation and oxidative stress are central to cancer development. Reducing these factors is perhaps the most important terrain correction of all. This is largely attainable through diet and lifestyle modifications:
- Adopt an Anti-Inflammatory Diet: What we eat can either fuel inflammation or fight it. Emphasize anti-inflammatory foods: high in natural omega-3 fatty acids, antioxidants, and low-glycemic nutrients. For example, fatty fish (like sardines, mackerel) or flaxseeds provide omega-3s which help balance pro-inflammatory omega-6 fats. A diet based on vegetables, fruits, whole grains, beans, nuts, and seeds is often referred to as a plant-based diet. It has been associated with lower levels of inflammatory markers in the body. These foods are rich in fiber. This fiber also helps feed good gut bacteria that produce anti-inflammatory compounds. They contain phytonutrients, like flavonoids and carotenoids, that directly neutralize free radicals. Curcumin (from turmeric) and gingerol (from ginger) are notable plant compounds. Green tea catechins are also notable. These compounds have shown anti-inflammatory and antioxidant effects, even in cancer models. They work by downregulating NF-κB and other inflammatory pathways [60]. In many African and Asian cultures, spices like turmeric, ginger, garlic, and chili are staple. Continuing their use can be protective. Increasing their use can also offer protection.
- Cut Down Pro-Inflammatory Foods: Reduce intake of processed and sugary foods, as well as processed meats. Diets high in refined starches and sugars cause spikes in blood sugar and insulin, promoting an inflammatory state. Processed meats and excess red meat have been linked to higher colorectal cancer risk. This is partly due to their pro-inflammatory effects and the presence of nitrosamines. If red meat is consumed, pair it with lots of vegetables and avoid charring it (charred meat contains carcinogenic compounds). Also, moderate the intake of omega-6-rich oils (like corn or soybean oil). Choose balanced oils like olive oil. Olive oil is high in anti-inflammatory monounsaturated fat and polyphenols. Essentially, shifting towards a whole-foods diet and away from “Western” processed foods will naturally decrease inflammation.
- Maintain Healthy Weight: Fat tissue, especially around the abdomen, produces pro-inflammatory cytokines like IL-6 and TNF-α. By maintaining or moving towards a healthy weight, one can markedly reduce these inflammatory signals. In breast cancer survivors, for example, those who lose excess weight have been found to lower recurrence rates, which is attributed partly to reduced inflammation and hormonal changes. Weight loss (if overweight) should be gradual and through diet and exercise, as described above. In populations undergoing lifestyle transition (urbanization, etc.), preventing obesity via community education on diet and physical activity is key.
- Be Active: Exercise isn’t just for immune and lymph – it also directly lowers inflammation in the long run. Regular exercise has been shown to reduce levels of C-reactive protein (CRP) and other inflammatory mediators. It also enhances antioxidant enzyme production in the body. Over time, an active person’s cells accumulate fewer DNA damage because of improved antioxidant defenses. Even walking 30 minutes a day can make a difference. For instance, a study on breast cancer patients found that those who followed healthy lifestyle recommendations had a 37% lower risk of cancer recurrence. The study noted these individuals had a lower recurrence rate. These recommendations included exercise. They also had over 50% lower risk of death[61] [62]. This is likely partly because exercise and diet reduced inflammation and improved immune function.
- Avoid or Limit Environmental Pollutants: Chronic exposure to polluted air or water can keep the body in an inflammatory state. Where possible, use clean fuels (natural gas or electricity instead of wood/charcoal indoors), and proper ventilation when cooking. If you work in dusty or chemical-laden environments, use masks or protective equipment. Advocate for cleaner community environments (e.g., reducing industrial emissions) – these public health measures pay dividends in cancer prevention. Even smoking cessation falls here. Quitting smoking not only reduces direct carcinogen exposure. Also, systemic inflammation drops within weeks of quitting.
- Manage Chronic Conditions: If you have chronic inflammatory conditions (like autoimmune diseases, hepatitis, ulcerative colitis, etc.), working with healthcare providers to control these conditions is vital. For example, controlling H. pylori infection in the stomach with antibiotics can cure the ulcer inflammation and thereby reduce stomach cancer risk. Treating Hepatitis B or C with antivirals can greatly reduce liver inflammation and subsequent liver cancer incidence. For autoimmune diseases, using the appropriate therapies to achieve remission can remove that constant inflammatory burden from the body. This area illustrates how conventional medicine and terrain care overlap. Sometimes, medications like antiviral or anti-inflammatory drugs are necessary to reduce dangerous inflammation.
- Stress Reduction and Social Support: Interestingly, psychological stress can induce an inflammatory response in the body (via cortisol dysregulation). Chronic stress and loneliness are associated with higher levels of inflammatory cytokines. Conversely, good social support and mental health can reduce stress. Practices like meditation or prayer have been correlated with lower inflammation. Community and family support – something often strong in African cultures – can be leveraged as a healing force. Additionally, activities like spending time in nature or traditional dancing can relieve stress and possibly improve one’s inflammatory profile indirectly.
- Antioxidant Supplements (Where Appropriate): The best source of antioxidants is food. In cases of poor diet or increased need, supplements like vitamin C, vitamin E, or selenium can be considered. This should be done preferably under guidance, as some high-dose antioxidants might interfere with certain chemotherapies. For most people, a multivitamin-mineral can plug gaps. However, megadoses are usually not necessary if diet is good. Some specialty supplements like omega-3 fish oil or curcumin extracts have evidence for reducing inflammation. They can be considered as adjuncts. This is especially true if diet sources are limited.
Implementing these strategies can transform a terrain of chronic inflammation into one of relative harmony. Remember that these lifestyle changes synergize: for example, diet and exercise together provide more benefit than either alone. And the earlier in life they’re adopted, the better – though it’s never too late to change the soil. Even cancer survivors in their 50s or 60s who improve their diet and lifestyle can lower their risk of recurrence. Studies have shown this significant reduction in risk. [63] [64] .
Conclusion: Cultivating a Cancer-Resistant Terrain for Life
Cancer is a complex disease. One clear lesson from both modern research and traditional wisdom is evident. We must attend to the “terrain,” not just attack the “tumor.” A well-functioning terrain is crucial. It includes a vigilant immune system that functions actively and freely moving lymph that clears wastes. A robust liver detoxifies threats effectively. Additionally, maintaining a low-inflammatory, low-oxidative environment is essential. Such a terrain is hostile to cancer’s development. By contrast, a broken terrain is cancer’s playground. This holistic perspective does not replace conventional treatments when cancer does occur. Instead, it complements them. Ideally, it prevents cancer from gaining a foothold in the first place.
Focusing on terrain health is empowering and cost-effective for individuals and communities. This is especially true in African or other low-resource settings. Not everyone has access to advanced cancer therapies. Yet, everyone can strive to eat nourishing whole foods and stay active. They can also avoid known carcinogens (like tobacco), prevent infections, and foster supportive social connections. These actions strike at the root causes that make the body vulnerable to malignancy. Public health measures include vaccinations (HBV, HPV). These initiatives also encompass improving water and air quality and combating poverty so people can afford nutritious food. These are essentially terrain-level interventions on a societal scale. They reduce the overall cancer burden.
It’s worth noting that many traditional lifestyles inherently promoted a healthy terrain. Diets were based on fresh plant foods and herbs. People engaged in daily physical labor. Strong community bonds helped buffer stress.
In places where westernization has eroded these practices, some basics can be reintroduced. This will mitigate the rising cancer rates. For example, in African villages, people still consume indigenous greens, millet, and fermented foods. They are also physically active. This results in lower rates of the “modern” cancers compared to big cities adopting processed diets. Protecting and modernizing these positive traditions – blending them with scientific knowledge – offers a path to better health.
In the fight against cancer, think of terrain care as “weeding the garden and enriching the soil”. We remove what poisons the soil (toxins, chronic infections) and add what nourishes it (nutrients, healthy behaviors). By doing so, we create an internal environment where the seeds of cancer have a very hard time taking root. If cancer has already appeared, correcting terrain imbalances becomes even more crucial. These corrections help the body respond to treatments, prevent metastasis, and avoid relapse. The long-term victory against cancer won’t be won by drugs or surgeries alone. It requires a comprehensive approach that heals the entire ecosystem of the body.
In conclusion, focusing on immune support and lymphatic movement lays a strong foundation. Adding liver detoxification and controlling inflammation or oxidative stress reinforces cancer prevention. These steps support survivorship. It aligns with the old adage that “prevention is better than cure.” We tilt the odds in favor of health by restoring balance to our terrain. We do this through mindful lifestyle choices and evidence-based natural strategies. This is a message of hope and empowerment. We have more control than we might think over the “soil.” Cancer could either wither or thrive in this soil. Maintaining a healthy terrain is a lifelong journey. It pays dividends in energy and vitality. It builds resilience against not only cancer but many chronic diseases. Let’s cultivate that resilient terrain for ourselves and our communities, so that cancer finds no sanctuary in our bodies.
Sources:
- Swann JB, Smyth MJ. Immune surveillance of tumors. J Clin Invest. 2007;117(5):1137-46. (Evidence that the immune system identifies and destroys nascent tumor cells) [I] [II]
- Swann JB, Smyth MJ. (continued). (Higher cancer rates in immunosuppressed patients, demonstrating the importance of immune surveillance)[III]
- Heather Alexander, MD Anderson Cancer Center. Exercise and the lymphatic system. Focused on Health, Nov 2019. (Role of lymphatic system in removing toxins and abnormal cells; importance of movement for lymph flow)[IV]
- Wikipedia: Stewart–Treves syndrome. (Rare angiosarcoma caused by chronic lymphedema, illustrating lymphatic stagnation can lead to cancer) [V]
- Michigan Health & Wellness. Liver Health and Detoxification: Your Body’s Built-In Cancer Defense. 2023. (How liver overload weakens immune surveillance and increases cancer risk; importance of Phase I/II balance) [VI] [VII]
- Block KI, et al. Integrative approaches for cancer prevention and therapy. Semin Cancer Biol. 2015;35(Suppl):S276–S304. (Relapse often occurs after few months due to resistant cells; need for broad-spectrum approach) [VIII] [IX]
- Chen L, et al. Inflammation and tumor progression: signaling pathways and targeted intervention. Signal Transduct Target Ther. 2022;7(1):258. (Chronic inflammation creates immunosuppressive microenvironment favoring tumorigenesis) [X]
- Nishida A, et al. The Role of Inflammation in Cancer: Mechanisms of Tumor Initiation, Progression, and Metastasis. Cells. 2023;14(7):488. (Inflammatory microenvironment is a hallmark of cancer; links lifestyle factors with cancer via inflammation) [XI]
- Reuter S, et al. Oxidative stress, inflammation, and cancer: How are they linked? Free Radic Biol Med. 2010;49(11):1603-16. (Oxidative stress from chronic inflammation causes DNA mutations; ROS promote angiogenesis and metastasis) [XII]
- Cannioto R, et al. Adherence to cancer prevention lifestyle recommendations and outcomes in high-risk breast cancer. JAMA Netw Open. 2023;6(5):e2318048. (Healthy lifestyle – diet, exercise, etc. – reduced recurrence by 37% and mortality by 58% in breast cancer patients) [XIII][XIV]
- Cohen L, Jefferies A. Lifestyle and cancer: integrative perspectives. ASCO Post. May 25, 2018. (At least 50% of common cancers are attributable to lifestyle factors; these factors influence hallmarks of cancer like inflammation and immune evasion) [XV][XVI]
- Chang E (MD Anderson surgeon), Cleveland S (physical therapist). The Exercise and the lymphatic system article highlights the importance of healthy weight and exercise for lymphatic health. It also discusses obesity’s link to cancer via inflammation and lymph damage. [XVII].
🧭 Ready to Rebuild Your Terrain?
If this article resonated with you, you already know: healing is deeper than removing a tumor. It’s about restoring balance to your gut, liver, lymph, immune system — and your peace of mind.
As a Natural Health Guide, I work with clients across all stages. This includes everything from prevention to post-treatment recovery. I use accessible, food-based, and culturally grounded strategies. These strategies strengthen your terrain from the inside out.
📌 Whether you’re navigating chronic inflammation, cancer recovery, or simply want to take control of your health…
👉 Let’s walk the healing path together. Contact Us
Discover more from Mike Ndegwa | Natural Health Guide
Subscribe to get the latest posts sent to your email.