Most people know the obvious red flags for cancer: lumps, unexplained weight loss, or chronic pain. However, emerging evidence suggests that our body’s internal “terrain” can broadcast more subtle early warning signs of cancer risk long before any tumor is detectable.
In holistic health circles, the term terrain dysfunction refers to imbalances in the body’s systems and environment that may create fertile ground for cancer to develop. These dysfunctions are often overlooked in mainstream healthcare because they don’t point to a specific disease, yet they can set the stage for cancer over time.
This article explores five unconventional early warning signs rooted in terrain dysfunctions: low lymphocyte counts, chronic constipation, persistent low-grade inflammation, hormonal imbalances (like fibroids), and high viral loads (EBV, HPV) – and explains how each can contribute to the cancer process.
For each warning sign, we also highlight natural, accessible interventions to help restore balance (think fermented foods, lymphatic movement, sunlight, bitter herbs, and more). The goal is to blend scientific depth with clear insights, drawing on global research and offering tips relevant even in African or other low-resource health contexts.
Low Lymphocyte Counts: Immune Surveillance on Decline
Low lymphocyte levels (purple white blood cells) amid red blood cells can signal a weakened immune surveillance. Chronic lymphopenia has been linked to higher risks of illness and even cancer. [1]
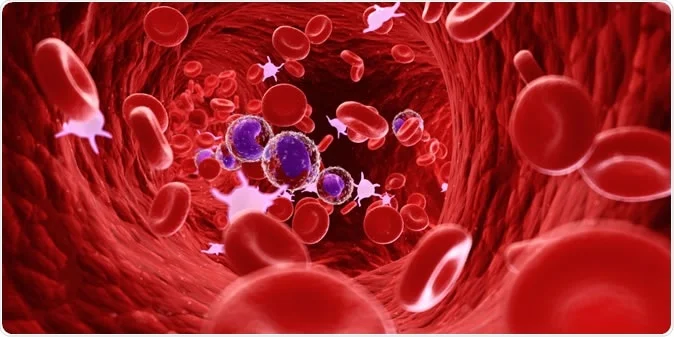
One of the body’s primary defenses against emerging cancers is the immune system – especially the lymphocytes, a type of white blood cell that includes T cells, B cells, and natural killer cells. These cells constantly patrol for abnormal or precancerous cells and destroy them before they become a problem. When lymphocyte counts are low (a condition called lymphopenia), this immune surveillance weakens.
Research has found that an incidental finding of low lymphocytes is associated with a 1.5- to 2.8-fold increase in risk of dying from cancer or other major diseases [2]. In other words, a persistently low lymphocyte count can be an early warning sign that the body’s cancer-fighting capacity is compromised.
Mainstream medicine often notices severe lymphopenia in the context of illnesses like HIV or during chemotherapy, but mild chronic lymphopenia in otherwise “healthy” individuals may be dismissed. This is an overlooked red flag: a terrain dysfunction indicating your internal environment might not readily catch nascent cancers.
Why would lymphocyte levels drop? Age is one factor (as part of aging, immune function can decline), as well as chronic stress or poor nutrition.
In some African and low-resource settings, chronic infections (like tuberculosis or untreated HIV) can quietly deplete lymphocytes, which in turn raises vulnerability to cancers such as Kaposi’s sarcoma or lymphoma [3]. Even without HIV, having continuously low lymphocytes means the immune system is less able to “see and seize” emerging cancer cells [4].
Experts believe reduced immune surveillance is a key reason why low lymphocyte counts predict higher cancer rates [5]. In fact, one large study of over 100,000 people found that people with low lymphocyte counts were significantly more likely to develop life-threatening illnesses in the future, including cancers [6].
In short, a weak immune terrain opens the door for cancer.
Natural Interventions to Strengthen Immunity: The encouraging news is that we can often improve our immune terrain with lifestyle measures:
- Nutrient-Dense Diet & Fermented Foods: Build up white blood cells by eating plenty of protein (for antibody and cell production) and micronutrients like zinc, selenium, and vitamins A, C, and E. Include fermented foods (yogurt, kefir, sauerkraut, kimchi, etc.) to nourish your gut microbiome – about 70% of the immune system resides in the gut, and a balanced microbiota helps regulate lymphocyte function. A healthy diet and balanced gut flora have been linked to better immune defense and could reduce cancer risk [7].
- Sunlight and Vitamin D: Safe exposure to sunlight boosts vitamin D levels, which are crucial for immune function. Vitamin D helps modulate lymphocytes and has been shown to enhance the body’s ability to fight infections and potentially surveil tumor cells [8] [9]. In many African communities, daily sun exposure is accessible and can improve vitamin D status, supporting immunity naturally.
- Lymphatic Movement & Exercise: Unlike blood, lymph fluid doesn’t have a heart to pump it; it relies on movement. Regular physical activity – brisk walking, dancing, skipping rope, even manual labor – acts as a natural pump for the lymphatic system. This lymphatic movement helps circulate immune cells throughout the body and clears out waste. Simple habits like rebounding (jumping on a trampoline) or doing jumping jacks can stimulate lymph flow. In low-resource settings, even without gym equipment, activities like carrying water, farming, or active household chores help keep the lymph system active.
- Herbal and Botanical Support: Several bitter herbs and medicinal plants are traditionally used to fortify immunity. For example, Moringa oleifera (drumstick tree) leaves – common in parts of Africa and Asia – are rich in vitamins and antioxidants that support white blood cell counts. Garlic, ginger, and turmeric are other accessible plants known to have immune-boosting and anti-inflammatory properties. Regularly incorporating these into meals or as teas can gently support immune vigilance.
- Stress Reduction and Sleep: Chronic stress and lack of sleep can significantly impair lymphocyte counts. Make time for stress-relief practices (prayer, meditation, deep breathing, community support) and aim for 7-8 hours of sleep, as these help the immune system regenerate. In any culture, rest and stress management are low-cost, critical tools to rebuild a vigilant immune terrain.
By proactively minding your immune terrain and addressing lymphopenia (even borderline cases) with these natural strategies, you improve your body’s chances of catching abnormal cells early and keeping cancer at bay.
Chronic Constipation: Gut Stasis and Toxic Exposure

Chronic constipation leads to prolonged stool retention (illustrated by pain in the colon), which may increase the contact time between potential carcinogens and the intestinal lining. Studies suggest managing constipation and maintaining a healthy gut can help reduce colorectal cancer risk. [10] [11]
Regular elimination is the body’s natural way of removing wastes and toxins, many of which could damage cells if they linger. Chronic constipation – typically defined as infrequent bowel movements or difficulty passing stool over a long period – is more than just an uncomfortable symptom. It represents a terrain dysfunction where the gut’s self-cleaning process is impaired. When stool sits in the colon for too long, potential carcinogens in the waste have extended contact with the intestinal lining [12]. For example, bile acids released during digestion can transform into secondary compounds that, if not promptly eliminated, may irritate and damage colon cells. Over months and years, this constant exposure to toxins can trigger mutations or promote an inflammatory environment in the colon – fertile ground for polyps and eventually colorectal cancer.
Scientific research has started drawing links between long-term constipation and higher rates of colon cancer. A recent analysis using genetic data suggested a potential causal link between chronic constipation and colorectal cancer [13] [14]. While the relationship is still being studied, the evidence is compelling: one conclusion was that “constipation could increase the risk of CRC (colorectal cancer)…making it a key risk factor”[15]. In practical terms, chronic constipation might be an early warning sign that your digestive “terrain” is out of balance and carcinogens are accumulating rather than being eliminated efficiently.
Mainstream healthcare often treats constipation as a minor complaint with laxatives, but rarely flags it as a cancer risk factor. Yet, addressing it early could be a form of cancer prevention. This is especially relevant in African and low-resource contexts where diets might be low in fiber and colorectal cancer rates are rising as lifestyles change. It’s empowering to know that by fixing constipation, you may also be cutting down your cancer risk [16] [17].
Natural Interventions for a Healthy Gut: Supporting healthy digestion and regular bowel movements can dramatically improve your terrain. Key strategies include:
- High-Fiber Foods: A diet rich in fiber adds bulk to stool and speeds up transit. Whole grains, legumes (beans, lentils), vegetables like okra or cassava leaves, fruits (especially with skins, like guava or pears), and local whole grains (maize, millet, sorghum) are excellent sources. Fiber not only relieves constipation but also binds possible carcinogens and excess hormones, carrying them out of the body. Research has shown that fiber intake is associated with lower colon cancer risk, likely by reducing contact between toxins and the colon wall [18] [19]. It can even lower estrogen levels in the body (more on that later) which is a bonus for reducing hormone-related cancer risks [20].
- Fermented and Probiotic Foods: Traditional fermented foods can be powerful allies for gut health. In many African cultures, staples like fermented millet porridge, yogurt, kefir, sauerkraut, or fermented cassava (gari) introduce beneficial bacteria. These probiotics help maintain a healthy gut microbiome which in turn supports regular motility and reduces inflammation. A balanced gut flora also produces short-chain fatty acids that nourish colon cells and may protect against cancer. In essence, fermented foods act as natural terrain conditioners for the colon.
- Hydration: In simple terms, water is the best laxative. Dehydration hardens stool and slows its passage. Drinking plenty of clean water (and clean herbal teas) throughout the day keeps the digestive tract lubricated. In areas where water is scarce or of concern, even broths or watery fruit like watermelon can contribute to hydration. Proper hydration, combined with fiber, ensures softer, bulkier stools that move quickly, minimizing toxin contact with your colon lining.
- Bitter Herbs and Digestive Aids: Bitter flavors stimulate digestion. Many cultures use bitter herbs to relieve constipation and improve liver and gallbladder function. For example, aloe vera bitters, senna leaf, or cascara have natural laxative compounds (though these should be used sparingly to avoid dependency). Gentler bitters like dandelion root, ginger, or lemon in warm water can kickstart digestive juices. In parts of Africa, chewing on bitter leaves (like Vernonia amygdalina, known as bitter leaf) is a folk remedy for stomach issues and could support bowel regularity. These remedies help by increasing bile flow and peristalsis (the wave-like gut contractions), addressing the sluggish terrain that causes constipation.
- Physical Activity and Massage: Sedentary lifestyles contribute to constipation. Regular movement – whether it’s walking to work, farming, or doing household chores – stimulates intestinal contractions naturally. In fact, cultures with squatting habits (for toileting or work) tend to have fewer issues with constipation, partly because squatting posture itself aids elimination. Simple abdominal self-massage, moving your hands in a clockwise circle around your belly, can also help move things along. These are low-cost, accessible techniques to support the body’s natural rhythm.
By treating chronic constipation not just as a nuisance but as a serious imbalance to fix, you detoxify your body’s terrain. The result is not only immediate comfort but also a long-term reduction in colon cancer risk – a significant benefit for such a simple lifestyle change [21].
Persistent Low-Grade Inflammation: The Slow Burn Toward Cancer
Inflammation is a normal immune response to injury or infection, but when it simmers at a low level for years, it can quietly do damage. Imagine a small, undying ember that never becomes a visible flame but slowly chars whatever it touches – that’s persistent low-grade inflammation in the body.
It’s a systemic terrain dysfunction often tied to modern lifestyles (poor diet, chronic stress, pollution, etc.), and it’s increasingly recognized as a fundamental driver of chronic diseases, including cancer [22]. In fact, scientists consider inflammation one of the hallmarks of cancer development [23].
Long before a tumor forms, pro-inflammatory cytokines (chemical messengers) can be wreaking havoc: they generate free radicals that damage DNA, promote excessive cell division, and create an environment where mutated cells can thrive and evade immune detection.
Many cancers arise at sites of chronic inflammation. For example, persistent hepatitis (liver inflammation) can lead to liver cancer, longstanding ulcerative colitis (colon inflammation) raises colon cancer risk, and chronic Helicobacter pylori infection in the stomach causing inflammation can lead to gastric cancer. But even without a diagnosed inflammatory disease, ongoing low-grade inflammation – marked by things like slightly elevated C-reactive protein (CRP) in blood tests, or vague symptoms like body aches, fatigue, or minor swelling – correlates with higher cancer incidence. One review noted that age-related chronic inflammation (“inflammaging”) likely contributes to the increased cancer rates seen in older adults [24]. Essentially, if your internal terrain is constantly irritated or “on fire” at a low level, normal cells in that environment are more likely to undergo malignant transformation over time [25]. Mainstream healthcare is starting to acknowledge this link; you’ll hear advice to eat anti-inflammatory diets for heart health or diabetes, which indirectly helps for cancer too. However, inflammation as an early cancer warning sign per se isn’t on most people’s radar. It should be, because addressing inflammation can significantly lower one’s cancer risk [26] [27].
So what causes these hidden inflammatory fires?
Often it’s lifestyle: diets high in sugar and processed foods, obesity (fat tissue secretes inflammatory signals), chronic infections, gum disease, or long-term stress.
In low-resource contexts, exposure to indoor smoke (from cooking fires), chronic parasitic infections, or persistent psychological stress of hardship can all keep the immune system in a constant, subtle state of alarm. You might not feel ill, but this chronic irritation is silently fueling DNA damage and cell changes.
The good news is that low-grade inflammation is reversible with consistent, natural approaches.
Natural Anti-Inflammatory Strategies: Cooling the internal fires of inflammation doesn’t necessarily require expensive drugs – many everyday foods and habits are potent anti-inflammatories:
- Whole Foods and Plant-Based Diet: An anti-inflammatory diet emphasizes whole, unprocessed foods, particularly plant foods. Vegetables and fruits provide antioxidants that neutralize free radicals. For example, brightly colored produce (berries, leafy greens, carrots, beets) are rich in flavonoids and carotenoids that lower inflammation. Whole grains and legumes deliver fiber that feeds good gut bacteria; a healthy gut lining prevents inflammatory toxins from leaking into the body. Traditional diets in many African and Asian communities – rich in greens, tubers, beans, and with minimal processed sugar – historically kept inflammation low. Embracing those dietary patterns today can restore that balance. Studies indeed show that plant-based diets contain many components that suppress inflammation and reduce cancer risk [28].
- Healthy Fats: Omega-3 and Olive Oil: Replace pro-inflammatory oils and fats (like fried foods, sunflower/corn oil, trans fats) with anti-inflammatory fats. Omega-3 fatty acids, found in flaxseeds, chia seeds, walnuts, and oily fish (sardines, mackerel), directly reduce inflammatory cytokine production. Likewise, extra virgin olive oil – a cornerstone of the Mediterranean diet – contains oleocanthal, a compound with effects similar to ibuprofen in tempering inflammation. These fats help bring the body back to equilibrium. Populations with high omega-3 intake (e.g. coastal communities eating a lot of fish) often show lower rates of inflammatory illnesses.
- Spices and Bitter Herbs: Your spice rack can be a medicine cabinet. Turmeric (with its active component curcumin) is a powerful anti-inflammatory – it’s been shown to downregulate inflammatory pathways and is being studied for cancer prevention. Likewise, ginger, cinnamon, and garlic can all help reduce inflammation. In many African herbal traditions, bitter tonics made from neem, artemisia, or African willow are used to “clean the blood” – likely reflecting their inflammation-lowering effects. Regularly brewing anti-inflammatory teas (like moringa leaf tea or hibiscus which is high in antioxidants) and cooking with spices can steadily lower chronic inflammation in the terrain.
- Moderate Sunlight Exposure: While excessive sun can cause skin issues, moderate sunlight has anti-inflammatory benefits, mainly through vitamin D synthesis. Vitamin D helps regulate the immune response and can prevent it from overreacting into a chronic inflammatory state [29] [30]. Ensuring adequate vitamin D (through sun or supplements) is linked to lower levels of inflammatory markers. It’s no coincidence that autoimmune and inflammatory issues often flare when vitamin D is low. For communities in Africa with abundant sunshine, harnessing that resource safely (short daily exposure of arms and legs) can improve vitamin D status and tame inflammation naturally.
- Stress Management and Sleep: Chronic stress is like gasoline on the fire of inflammation – it keeps cortisol and adrenaline high, which over time dysregulates the immune system and promotes an inflammatory milieu [31]. Practices such as mindfulness, prayer, deep breathing exercises, or yoga can signal the body to shift into “rest and repair” mode, dialing down inflammatory stress responses. Equally important is sufficient sleep. During deep sleep, the body clears out inflammatory toxins (for example, the brain removes waste via the glymphatic system at night). People who sleep poorly have higher levels of inflammation; prioritizing 7-9 hours of quality sleep is a simple, free anti-inflammatory “therapy” that also boosts overall cancer-fighting capacity.
- Regular Physical Activity: Exercise is one of the most potent, yet accessible, anti-inflammatories. When we engage in moderate activity, our muscles release anti-inflammatory substances (like IL-10 and myokines) that counteract inflammation throughout the body. Communities that maintain an active lifestyle – whether through manual farming, walking long distances, or regular dancing – inherently keep inflammation in check. Aim for at least 30 minutes of moderate activity most days (in whatever form is enjoyable and feasible) to continuously extinguish those inflammatory embers.
In summary, low-grade inflammation is a silent spark that can ignite cancer, but it’s also a spark we can smother with consistent lifestyle choices. As one expert put it, an anti-inflammatory lifestyle (good diet, exercise, stress reduction) “holds strong potential to reduce cancer risk”[32]. By tending to this aspect of your terrain, you’re not just improving how you feel day-to-day (more energetic, less achy), but also making your body a much more hostile place for cancer to ever gain a foothold.
Hormonal Imbalances and Fibroids: Estrogen’s Influence on Terrain
Hormones are powerful messengers that regulate growth and repair in our bodies. When they fall out of balance, they can create a terrain that nudges cells toward unchecked growth.
A common but often overlooked sign of hormonal imbalance in women is the development of uterine fibroids (benign tumors of the uterus). Fibroids themselves are non-cancerous and almost never turn malignant [33].
However, fibroids thrive on a hormonal terrain dominated by estrogen and related growth signals. Think of fibroids as a warning light: they indicate that estrogen (and often insulin and other growth factors) has been consistently high or unopposed by progesterone, leading uterine muscle cells to grow into benign tumors.
This estrogen-dominant environment doesn’t just affect the uterus – it can also set the stage for hormone-dependent cancers like certain breast cancers or endometrial (uterine lining) cancer if not corrected.
How are fibroids and cancer risk connected?
While fibroids do not turn into cancer, the conditions that allow fibroids to grow can also fuel cancerous growths.
High estrogen levels, especially when not balanced by progesterone (as can happen in PCOS or perimenopause), are a known risk factor for cancers of the breast and uterus [34].
One study found that women with a history of fibroids had a slightly higher risk of breast cancer, suggesting a common underlying hormone terrain [35].
Excess estrogen can stimulate cells in the breasts or uterine lining to proliferate more than normal, increasing the chance of a rogue cell forming a tumor.
Additionally, estrogen can interfere with DNA repair mechanisms in cells, compounding the risk when exposure is long-term.
Mainstream medicine typically treats fibroids with medication or surgery and might reassure patients that fibroids are benign (which is true). What’s often missed is the bigger picture – fibroids are like a big billboard announcing that your hormone balance is off-kilter in a way that, if persistent, could encourage cancerous changes down the line.
This terrain issue isn’t limited to women; men too can have hormonal imbalances (for instance, high estrogen or low testosterone environments have been linked to prostate problems). But fibroids in women offer a very tangible early warning sign.
In African and African-descendant populations, fibroids are especially common (due to a mix of genetic and environmental factors), often appearing at younger ages and in greater numbers. This means the message of fibroids as a red flag is particularly relevant in African contexts – it’s an opportunity to take stock of hormonal health early.
Furthermore, low-resource settings might not have widespread screening for breast or endometrial cancer, so recognizing and addressing hormonal dysfunctions proactively is a crucial prevention strategy.
Natural Hormone-Balancing Interventions: The good news is that hormones respond well to lifestyle adjustments and natural therapies. To recalibrate an estrogen-dominant (or otherwise imbalanced) terrain:
- Fiber and Flax for Estrogen Balance: We mentioned fiber in the context of constipation, but it plays a starring role in hormone health too. A high-fiber diet helps bind and remove excess estrogens that the liver dumps into the gut for excretion [36]. If you’re not getting enough fiber, those estrogens can get reabsorbed into circulation, perpetuating high levels. Ground flaxseed is a fantastic fiber source with added benefits: it contains lignans, compounds that have gentle estrogen-modulating effects (they can weakly bind to estrogen receptors, blocking stronger estrogens). Some studies suggest flaxseed in the diet is associated with lower risk of breast cancer, likely due to these properties. Locally available fiber heroes include okra, whole grains, beans, pumpkin leaves, and fruits like pawpaw (papaya). By keeping bowel movements regular and flush with fiber, you lighten the estrogen load on your tissues.
- Cruciferous Vegetables and Bitter Greens: Veggies like broccoli, cabbage, kale, cauliflower, and African bitter leaf are not just nutritious – they contain specific phytochemicals (indoles like I3C and sulforaphane) that help the body metabolize estrogen into safer forms. Essentially, they tilt estrogen processing away from the more carcinogenic metabolites towards benign ones. These vegetables are often bitter or pungent, which in herbal traditions is a sign of their liver-supportive properties. The liver is our hormone detox factory, and bitter foods/herbs (like dandelion greens, neem, artichoke, turmeric) support liver enzymes that break down excess hormones. For women with fibroids or heavy estrogen signs (like cyclic breast tenderness), a daily serving of these cruciferous or bitter greens can be therapeutic over time, helping to shrink fibroids and reduce cancer-risk estrogens.
- Maintain Healthy Weight & Blood Sugar: Fat tissue produces estrogen (specifically, it converts adrenal hormones into estrogen). So, carrying a lot of excess weight can feed an estrogen-dominant terrain. Moreover, high insulin from insulin resistance (often diet-induced) can stimulate ovaries to make more estrogen and can directly encourage cell growth. By aiming for a healthy weight through diet and exercise, you reduce those hormonal growth signals. This doesn’t mean becoming skinny – rather, focus on fat loss if overweight, and improving insulin sensitivity by cutting down on sugar and refined carbs. In many communities, adopting more traditional starches (like sweet potatoes, yams, unrefined maize) instead of sugary drinks and processed foods can make a big difference. The result is often a natural correction in hormone levels and less stimulation for both fibroids and potential tumors.
- Herbal Allies for Hormone Harmony: Various cultures have fertility or menstrual herbs that incidentally aid hormone balance. For example, black cohosh and chasteberry (Vitex) are used to regulate cycles and can help recalibrate estrogen-progesterone balance (though these might be less accessible in some regions). In African herbal medicine, ngumba (Kigelia africana) and turmeric are sometimes used for fibroid relief – turmeric, in particular, has research-backed anti-estrogenic and anti-inflammatory effects on uterine cells. Bitter melon and fenugreek (commonly used for blood sugar) also have hormonal benefits. Always approach potent herbs with guidance, but know that nature offers many options to nudge hormones in the right direction. Even simple ginger and garlic, by reducing inflammation, indirectly aid hormone signaling pathways to normalize.
- Sunlight and Vitamin D: Interestingly, vitamin D isn’t just for bones and immunity – it also plays a role in gene regulation in fibroid and breast tissue. Studies have found that women with sufficient vitamin D levels have a lower incidence of fibroids, and vitamin D can slow fibroid cell growth in lab studies. Our skin makes vitamin D from sunlight, so getting regular sun (while avoiding burns) is a natural way to optimize this hormone-like vitamin. For darker-skinned individuals (more common in Africa), a bit more sun exposure is needed to generate the same vitamin D, so ensure you get a good dose of morning or late afternoon sun when UV is moderate. Vitamin D’s balancing effect on cell growth extends to potentially lowering cancer cell proliferation in breast and colon tissue as well. In short, sunlight in appropriate amounts can be a hormonal tonic.
- Mindful Use of Plastics and Chemicals: Our environment is awash with endocrine disruptors – chemicals that mimic or interfere with hormones. Plastics, pesticides, and certain cosmetics contain compounds (like BPA, phthalates, parabens) that can act like estrogen in the body. Reducing exposure can help lighten the estrogenic burden. This might mean using glass or stainless steel for food storage instead of plastic, choosing natural beauty products, and favoring organic foods or thoroughly washing produce to remove pesticide residues. In low-resource settings, it can be as simple as not reusing plastic bottles in the sun (heat releases more chemicals) and ventilating your home when using insecticides or chemical cleaners. Protecting your terrain from these synthetic hormones creates a cleaner slate for your body’s own hormones to balance out.
By heeding the warning of fibroids and related hormonal symptoms, you can take proactive steps that not only shrink those benign growths but also lower your risk for hormone-driven cancers.
The key is to view fibroids (or even symptoms like long, heavy menstrual cycles, severe PMS, etc.) as messages from your body that the hormone environment needs support. Balancing that terrain with the above strategies leads to healthier breasts, ovaries, uterus – and indeed, a healthier you overall.
Chronic Viral Loads (EBV, HPV): When Infections Linger and Fuel Cancer
We usually think of infections as short-term events – you get sick, you recover, end of story. But some viruses have a lifelong relationship with us and can contribute to cancer in the long run if our immune “terrain” doesn’t keep them in check.
Two of the most noteworthy in this category are Epstein-Barr Virus (EBV) and Human Papillomavirus (HPV).
These viruses are incredibly common (EBV infects ~90% of people globally, HPV infects most sexually active people at some point [37] [38]), and in the majority they stay quiet or cause only minor issues.
However, when they remain active or at high levels (high viral load) in the body over time, they can set the stage for cancer by inserting their genes into our cells or by causing chronic inflammation.
HPV is the clearest example: certain “high-risk” strains of HPV cause persistent infections in the cervix (as well as throat, anal, and penile tissues) and can directly trigger cells to become cancerous.
In fact, persistent high-risk HPV infection is the cause of virtually all cervical cancer cases [39]. If the immune system doesn’t clear HPV within about 1-2 years, the virus can induce precancerous changes that may progress to cancer over 10-15 years [40] [41]. This is why Pap smears and HPV tests look for signs of lingering HPV effects.
An untreated persistent HPV infection is essentially a blinking warning sign that cancer could develop down the road.
Unfortunately, in many low-resource settings, routine screening is limited – which is part of why cervical cancer remains the leading cause of cancer death among women in sub-Saharan Africa [42].
The terrain message here is that a high viral load of HPV is a serious red flag – not a cause for panic, but a call to strengthen immunity and pursue interventions (medical or natural) to eradicate or control the virus before it causes harm.
EBV, on the other hand, is a master of hiding in our B cells.
Most people get EBV (often as harmless mono or “kissing disease” in youth) and never have issues. But if the virus reactivates chronically or the immune system can’t keep a lid on it, EBV can contribute to cancers like certain lymphomas and nasopharyngeal carcinoma.
EBV is classified as a Group 1 carcinogen for humans – it’s definitively linked to cancer development in some cases [42]. For instance, EBV is found in about 40% of Hodgkin lymphoma cases and almost all cases of endemic Burkitt lymphoma [43].
In African regions where malaria is common, the combination of EBV infection with chronic malaria in children is the main risk factor for Burkitt lymphoma. Malaria weakens immune control of EBV, allowing EBV-infected B cells to proliferate unchecked, which can lead to lymphoma. So, a high EBV load (or frequent reactivation indicated by symptoms like chronic swollen glands or high EBV titers in blood tests) is a terrain dysfunction signifying a stressed immune system that’s losing grip on a cancer-linked virus.
EBV may also play a role in some stomach cancers and nasopharyngeal cancers [44]. While these EBV-related cancers are relatively rare, they illustrate how a normally latent virus can become a carcinogenic threat when terrain conditions permit (e.g., co-infections, immune suppression, genetic susceptibility).
Mainstream healthcare does acknowledge HPV and EBV in relation to cancer – HPV testing is common in women’s health, and doctors know EBV can cause lymphoma in immunosuppressed patients.
However, outside those contexts, high viral loads are often not on the radar as a general early warning. You won’t get a “viral load” report in a typical checkup. But if you happen to know you have chronic HPV or EBV issues (or other viruses like hepatitis B/C or HIV, which also elevate cancer risk), it’s crucial to see this as a modifiable risk factor.
Strengthening your terrain to suppress these viruses can literally be lifesaving.
Natural Antiviral and Immune Strategies: The goal is to support your immune system to do what it does best – keep viruses latent or eradicate them if possible. Some accessible interventions include:
- Optimize Nutrient Status: Certain nutrients are particularly important for antiviral immunity. Vitamin C, zinc, and selenium stand out. Vitamin C-rich foods (citrus, guava, bell peppers, leafy greens) bolster white blood cell function against viruses. Zinc (found in seeds, lentils, meat) is crucial for developing T cells and NK cells that target virus-infected cells; zinc deficiency is common where diets lack diverse protein and can lead to weaker antiviral immunity. Selenium, found in grains, nuts (especially Brazil nuts), and fish, helps the body produce powerful antioxidant enzymes that prevent viral damage. In Africa, soils are sometimes low in selenium, making dietary intake subpar – so seeking out selenium-rich foods or using a multivitamin can help. Ensuring a diet with ample vitamins and minerals essentially arms your immune soldiers to suppress viruses like HPV and EBV more effectively.
- Herbal Antivirals and Bitter Tonics: Nature provides many antiviral herbs that have been used in traditional medicine. For HPV, some studies have looked at green tea extracts (EGCG) which, applied topically or taken orally, can help regress cervical dysplasia by its antiviral and anti-tumor effects. Green tea is rich in catechins and is accessible in many places now – even if not traditionally used in Africa, it can be imported or grown in some regions. Garlic is a broad-spectrum antimicrobial; its component allicin can help fight viruses and is known to boost immunity. Regularly eating raw or cooked garlic is a folk remedy for infections that has some scientific backing. Medicinal mushrooms like reishi, turkey tail, or shiitake contain beta-glucans that rev up virus-fighting cells – these might be less available in some areas, but where they are, they can be a great immune tonic. Bitter herbs, used often for “blood cleansing,” can stimulate immune function too; for example, Andrographis paniculata (known as “King of Bitters” in Asia) has shown antiviral activity against Epstein-Barr in lab studies. In West Africa, extracts of bitters like neem or moringa are traditionally taken for malaria and infections – these could potentially aid in keeping EBV at bay indirectly by improving overall immune response.
- Lymphatic Movement and Detoxification: To help your immune system target viruses, it’s important to keep your internal environment clean and flowing. We’ve touched on exercise’s role in immunity and lymph circulation. Here it’s worth emphasizing sweating and detoxification. When you exercise or do activities that induce a mild sweat, you may help expel toxins and byproducts of infection. Some viruses like to hide in tissues; gentle heat stress from exercise or even traditional practices like sitting in a sauna (or simply a steamy bath) can support circulation and immune cell trafficking. In tropical areas without saunas, a brisk walk under the sun or manual field work can induce a healthy sweat. Just be sure to hydrate and replace electrolytes (coconut water, homemade oral rehydration solutions, etc.). Regular movement ensures immune cells are distributed everywhere and can chase down viruses in lymph nodes or organs before they cause mischief.
- Sunlight and Restful Sleep: We circle back to these because they are fundamental. Sunlight, through vitamin D, again plays a role – higher vitamin D levels are associated with lower risk of viral reactivation (some observational studies even found people with better vitamin D have less HPV persistence and fewer EBV-related issues). Also, UV light itself can kill viruses on surfaces and possibly on the skin, though you wouldn’t rely on that internally. More importantly, sleep is when the immune system is highly active in surveillance mode. During deep sleep, certain immune cells (like cytotoxic T cells) become more active, and inflammatory cells less so. Prioritizing sleep is thus crucial for giving your body time to hunt down cells harboring EBV or HPV-infected cells in the cervix and eliminate them. In traditional cultures, the sundown to sunup sleep pattern supported immunity; modern life has shortened sleep, which can lead to higher susceptibility to chronic infections. Making an effort to synchronize with natural day-night cycles (circadian rhythm) can enhance antiviral immunity.
- Medical Integrations: While this article focuses on natural interventions, it’s worth mentioning accessible medical tools: HPV vaccination is a powerful prevention method for the strains that cause most cervical cancers. Many African countries are increasing access to the HPV vaccine for young girls (and boys in some cases); it’s a science-backed way to prevent a terrain dysfunction (persistent HPV infection) from ever taking hold. If you have children or grandchildren, supporting vaccination programs can change the landscape of cervical cancer in the coming generations. For EBV, there is no vaccine yet, but treating co-factors like controlling malaria in endemic regions (using bed nets, antimalarial treatments) indirectly reduces EBV-related cancer risk [45]. Also, if someone is living with HIV (another chronic virus that weakens immunity and raises cancer risk), adherence to antiretroviral therapy (ART) will keep the immune system stronger to suppress other viruses – a great example of blending natural support (nutrition, etc.) with medical treatment for terrain benefit.
In summary, chronic or high viral loads of EBV, HPV, and other oncogenic viruses act as silent saboteurs in the body’s terrain. They often fly under the radar until a cancer appears. But with vigilance (through screening where possible) and proactive strengthening of the immune environment, you can keep these viruses dormant or eradicate them. It’s a testament to how intricately infection and cancer are linked – and how nurturing a resilient terrain can break that link.
As Cancer Research UK succinctly notes, “Some infections increase the risk of cancer, including EBV, HIV, hepatitis, and parasites” [46]: yet for each of those, there are preventative strategies. By managing the viral piece of the terrain puzzle, you remove one more big risk factor from the cancer equation.
Conclusion: Cultivating a Cancer-Resistant Terrain
Cancer doesn’t usually appear overnight – it’s the culmination of cells responding to years of signals from their environment. Your body’s terrain – the immune strength, the inflammatory tone, the hormonal milieu, the presence of toxins or viruses – is the soil in which either healthy cells or cancerous cells can flourish.
The early warning signs discussed here are like signals of bad weather for that soil. Low lymphocyte counts warn of weak immune defenses; chronic constipation points to toxin buildup and a strained gut; persistent low-grade inflammation denotes ongoing damage; fibroids signal hormonal excesses; and high viral loads reveal a compromised hold over latent threats.
The encouraging message is that each of these terrain dysfunctions is addressable. By listening to these whispers and correcting course, we can often avoid the shout of a full-blown cancer diagnosis later.
In practical terms, an evergreen cancer-prevention strategy emerges from this discussion:
- Support your immunity every day – through nutrition, movement, and stress management – so that low lymphocytes or sluggish defenses are reversed before malignancies take advantage.
- Prioritize elimination and detoxification – daily bowel movements, sweating, clean water – to reduce the contact time your cells have with any carcinogens.
- Soothe the chronic inflammation – with wholesome food, herbs, exercise, and adequate sleep – recognizing that a cool internal environment is hostile to cancer.
- Balance your hormones naturally – via diet, weight management, and perhaps herbal help – appreciating that hormonal harmony protects against uncontrolled growths.
- Be vigilant against chronic infections – use available vaccines, traditional remedies, and immune boosters – to ensure viruses and other microbes are not allowed to continuously provoke or alter your cells.
These interventions – fermented foods, lymphatic exercise, sunshine, bitter herbs, and other accessible remedies – are not fanciful folk tales but grounded in scientific insight and endorsed by expert observations. They are globally informed yet locally actionable.
For instance, the idea that a high-fiber diet can reduce estrogen and colon cancer risk is supported by Harvard research [47], but it can be executed with local foods like millet, beans, or greens available in an African village.
The concept that ongoing inflammation raises cancer risk is accepted in top scientific journals [48], and the solution might be as simple as cooking traditional anti-inflammatory recipes with turmeric and garlic, or going for a daily walk at sunset.
By viewing health through this “terrain” lens, we shift from a reactive stance (waiting for disease to strike) to a proactive one.
It’s a hopeful message: the power to prevent cancer may lie in consistently tending the soil of our well-being.
Modern medicine rightly focuses on treating disease, but as individuals and communities, we can focus on cultivating health. This synthesis of scientific depth and common-sense natural wisdom aims to guide you in that journey.
Remember, the body communicates early and often – subtle signs like those we’ve discussed are invitations to course-correct. Heed them, respond with even small changes, and you stack the odds in favor of long, cancer-free vitality.
Your terrain, your rules.
Here’s to creating an inner environment where cancer simply cannot take root.
Sources:
- Laguipo, A.B. (2020). Lymphopenia may hint a higher risk of future illness, death. News-Medical.Net. [i] [ii]
- Bonavitacola, J. (2023). Potential Link Exists Between Constipation, Colorectal Cancer. AJMC. [iii] [iv]
- Harvard T.H. Chan School of Public Health (2020). High-fiber diet linked with reduced breast cancer risk. [v]
- Divella, R. et al. (2020). Lifestyle as a modulator of low-grade inflammation in cancer. Clinical Nutrition ESPEN. [vi]
- Cancer Research UK (2021). Infections (e.g. HPV) and cancer: EBV, HIV, hepatitis. [vii] [viii]
- World Health Organization (2024). Human papillomavirus (HPV) and cancer Fact Sheet. [ix]
- Cancer Research UK (2021). Does Epstein-Barr Virus cause cancer?. [x]
- Ngugi, C.W. et al. (2011). Persistent HPV infection and cervical cancer risk in Africa. Journal of Epidemiology. [xi] [xii]
- Onyango, J. et al. (2022). Malaria, EBV and endemic Burkitt Lymphoma. Infectious Agents and Cancer. [xiii]
If this article sparked something in you — a realization, a concern, or even hope — don’t ignore it. The terrain can be restored. The earlier, the better. As a Natural Health Guide, I help individuals understand their body’s signals, reverse dysfunction through food and daily rhythm, and rebuild a strong, cancer-resistant foundation using what nature has already provided. If you’re ready to stop guessing and start healing with intention, I’m here to walk with you.
📲 Reach out: Contact Us
Let’s rebuild your terrain — before disease ever takes root.
Discover more from Mike Ndegwa | Natural Health Guide
Subscribe to get the latest posts sent to your email.